Chapter 28
Choroidal Drainage
Choroidal detachments can be serous, hemorrhagic, or a mixture of both.
Serous choroidal detachments often occur in the setting of post-operative hypotony (Figure 28.1). This is most commonly secondary to wound leakage such as following glaucoma surgery but can also be due to ciliary body shutdown.[1,2] In most cases, serous choroidal effusions will settle spontaneously and do not require drainage. Leaking wounds should generally be sutured closed, although sometimes a bandage contact lens can be considered with close observation.
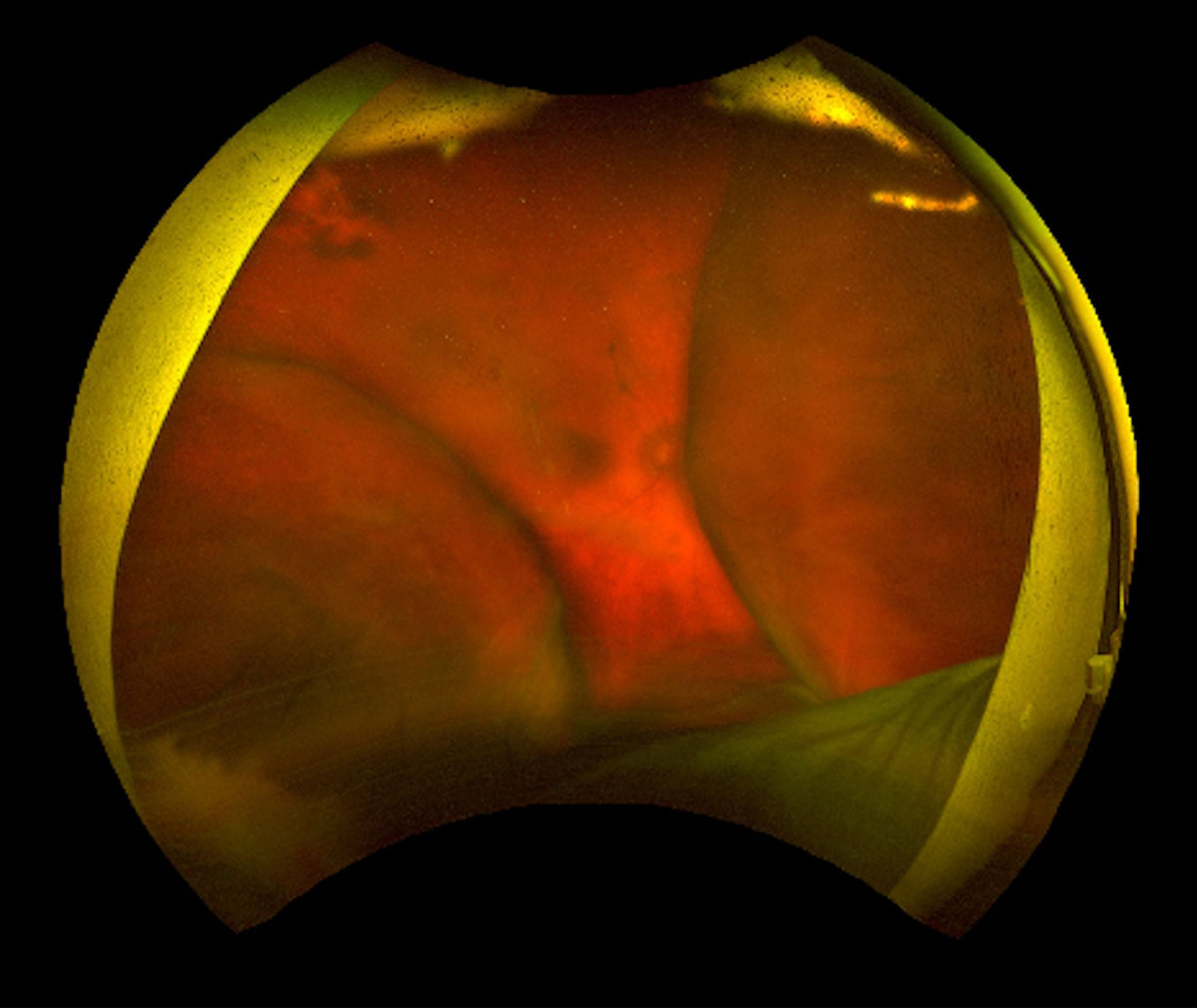
Hemorrhagic choroidal detachment can occur spontaneously or more commonly following an episode of acute intra-operative hypotony (Figures 28.2-5) Systemic risk factors include older age, increased venous pressure from a Valsalva maneuver such as coughing, systemic hypertension, blood dyscrasias such as thrombocytopenia and the use of antiplatelets or anticoagulants. Intraocular risk factors include high myopia, hypotony, glaucoma, and choroidal lesions, such as hemangiomas and melanoma.[3,4]
Ying S, Sidoti PA, Panarelli JF. Risk factors and management of choroidal effusions. Curr Opin Ophthalmol. 2023;34(2):162-7.
Mantopoulos D, Hariprasad SM, Fine HF. Suprachoroidal Hemorrhage: Risk Factors and Diagnostic and Treatment Options. Ophthalmic Surg Lasers Imaging Retina. 2019;50(11):670-4.
Honig SE, Srinivasan A, Shields CL. Suprachoroidal Hemorrhage Simulating Melanoma in Idiopathic Thrombocytopenic Purpura. Ocul Oncol Pathol. 2019;5(3):162-6.
Marous CL, Sioufi K, Shields CL, Mashayekhi A, Shields JA. COUGHING-INDUCED SUPRACHOROIDAL HEMORRHAGE SIMULATING MELANOMA IN TWO CASES. Retin Cases Brief Rep. 2018;12(4):336-41.
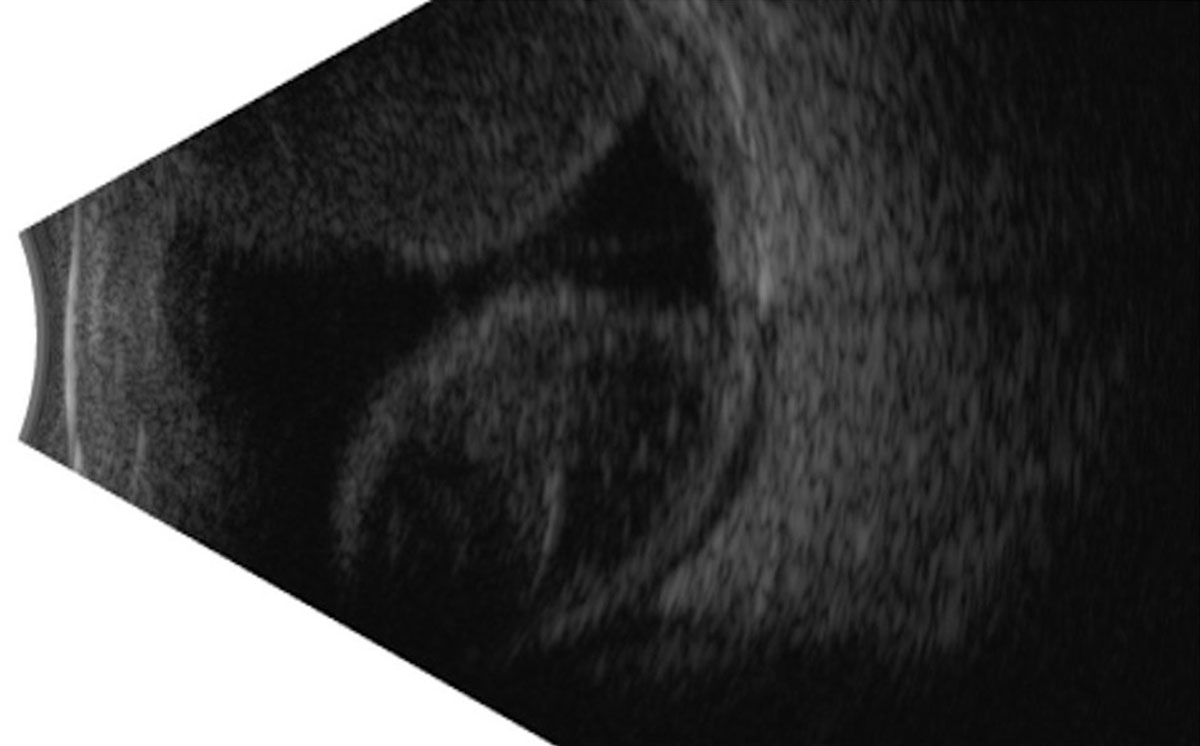
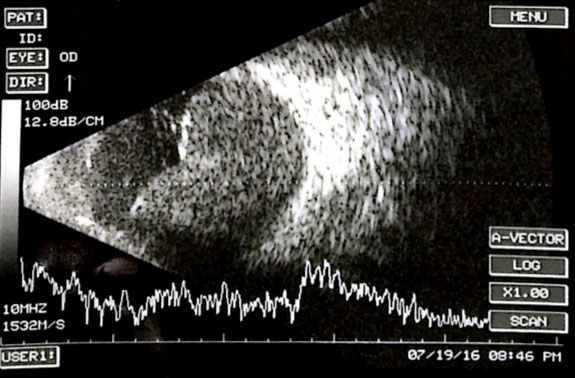
Figure 28.2 B
B-scan ultrasound showing the same.
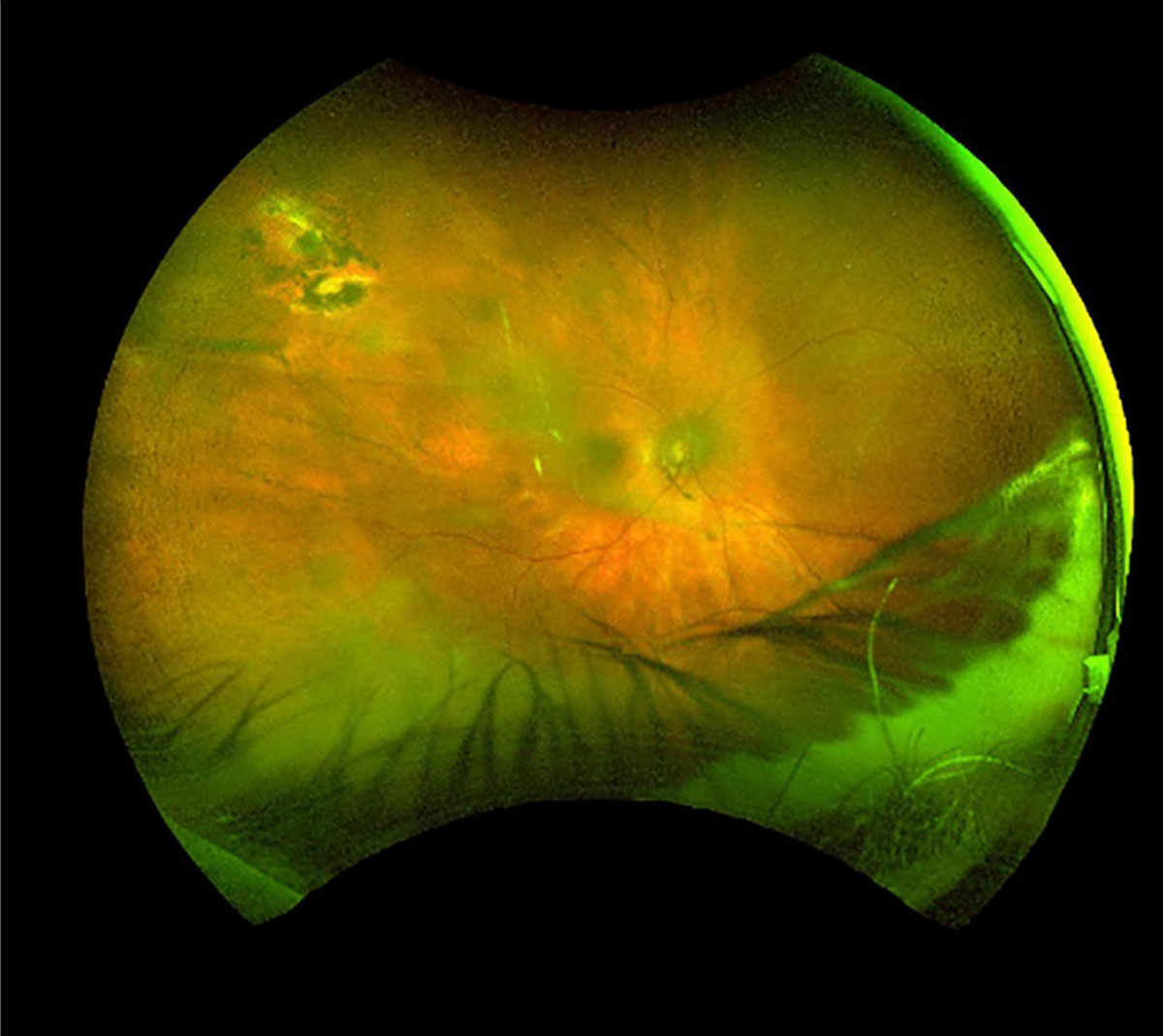
Figure 28.2 C
Complete resolution of the suprachoroidal hemorrhage after 6 weeks of medical management. The patient’s visual acuity returned to baseline without surgical intervention.
In non-appositional cases, surgical and conservative approaches with frequent monitoring of hemorrhage absorption using B-scan ultrasonography have been well described.[5]
In cases of spontaneous hemorrhagic choroidal detachment, a blood count should be ordered to rule out thrombocytopenia or other blood disorders that may need to be managed. If the patient is taking antiplatelet or anticoagulant medications, discussion with their physician can help determine if these can be safely ceased or the dose reduced.
The use of periocular or sub-Tenon steroids can help reduce the inflammatory cascade following the hemorrhage and play a role in platelet activation to prevent rebleeding.[6]
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Westmead Eye Manual
This invaluable open-source textbook for eye care professionals summarises the steps ophthalmologists need to perform when examining a patient.